Chronic inflammatory demyelinating polyneuropathy
Polyneuropathy encompasses various immune-mediated neuropathies, including Guillain-Barré syndrome (acute) and chronic inflammatory demyelinating polyneuropathy (CIDP). Other types include CIDP variants, multifocal motor neuropathy, conditions like MGUS, POEMS syndrome, neuropathy with IgM gammopathy, and Waldenström macroglobulinemia. Also involved are mixed cryoglobulinemia syndrome, GALOP syndrome, CANOMAD syndrome, primary amyloidosis, paraneoplastic neuropathies, and neuropathies associated with systemic autoimmune diseases. These present with diverse sensory, motor, or autonomic symptoms, and treatment is typically specific to the underlying cause.
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP):
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired, immune- mediated neuropathy affecting peripheral nerves and nerve roots. CIPD is characterised by a relapsing- remitting or progressive course and electrodiagnostic or pathological features of demyelination. In its classic form, CIDP manifests as a symmetrical, motor- predominant neuropathy which results in both proximal and distal muscle weakness. CIPD variants include asymmetric sensorimotor (multifocal) and sensory-predominant forms. (1, 2)
Treatment with Corticosteroids
Treatment for CIDP includes corticosteroids such as, oral prednisolone in a dose of 1–1.5 mg/kg until improvement is maintained and then the dose is tapered until the lowest effective maintenance dose is reached. Alternatively, intravenous immunoglobulin (IVIG) has been proven to be effective and is often used as a treatment for the disease. IVIG has different brands. A suggested protocol for IVIG is with 400 mg/kg/day for 5 consecutive days with premedication with paracetamol 1gm, chlorphenramine , hydrocortisone 100mg IV. (3, 4)
Plasma Exchange (PE) in CIDP
Plasma exchange (PE) has also been shown to be of benefit in chronic inflammatory demyelinating polyneuropathy. Plasmapheresis is through removal of circulating antibodies, complement, and soluble biological response modifiers. Plasma exchange is usually given for four to six treatments over eight to 10 days. (5)
Other Immunosuppressive Agents
Additionally, other immunesuppressive agents, such as, azathioprine (2 mg/kg/day), mycophenolate mofetil , methotrexate (10 to 25 mg given once weekly suggested) may be considered for resistant cases. However, neither of these agents has proven efficacy. (6, 7)
Non-Pharmacological Measures
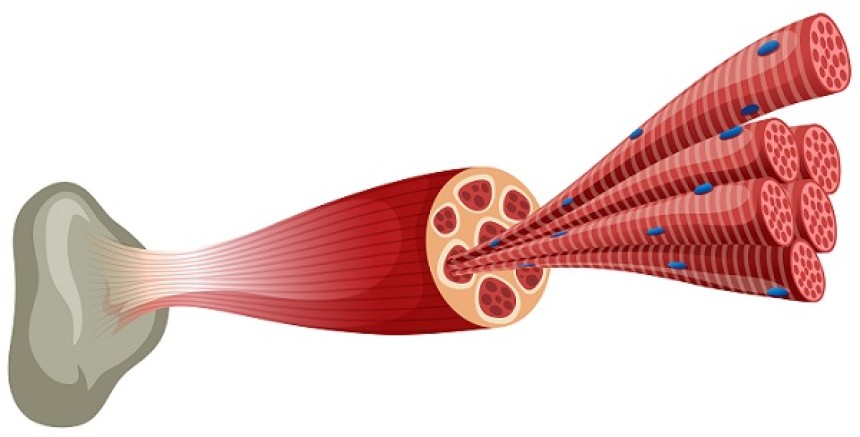
Non pharmacological measures including physical therapy may improve muscle strength, function and mobility, and minimise the shrinkage of muscles and tendons and distortions of the joints. (8)
References
1- Dalakas MC. Advances in the diagnosis, pathogenesis and treatment of CIDP. Nat Rev Neurol. 2011;16:507-17.
2-Villa AM, et al. Chronic inflammatory demyelinating polyneuropathy. Findings in 30 patients. Medicina (B Aires). 1999;59:721-6. Villa AM, et al. Chronic inflammatory demyelinating polyneuropathy. Findings in 30 patients. Medicina (B Aires). 1999;59:721-6.
3- Comi G, et al. Treatment of chronic inflammatory demyelinating polyneuropathy. Ital J Neurol Sci. 1998;19:261-69.
4- Kissel JT, The treatment of chronic inflammatory demyelinating polyradiculoneuropathy, Semin Neurol, 2003;23:169–80.
5-Lehmann HC, Hartung HP. Plasma exchange and intravenous immunoglobulins; mechanism of action in immune-mediated neuropathies. J Neuroimmunol. 2011;231:61-9
6-Joint Task Force of the EFNS and the PNS. European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society–First Revision.J Peripher Nerv Syst. 2010;15:1-9.
7- Gorson KC, et al. Chronic inflammatory demyelinating polyneuropathy: clinical features and response to treatment in 67 consecutive patients with and without a monoclonal gammopathy. Neurology. 1997;48:321-28.
8- Ryan MM, et al. Childhood chronic inflammatory demyelinating polyneuropathy: clinical course and long-term outcome. Neuromuscul Disord. 2000;10:398-406.