Multiple sclerosis RRMS Latest Diagnostic criteria
Relapsing-remitting MS (RRMS) is diagnosed clinically, typically presenting in young adults with episodes of CNS dysfunction, such as vision loss or limb weakness. MRI reveals characteristic hyperintense white matter lesions. The McDonald criteria aid diagnosis, requiring evidence of multiple attacks and lesions. Additional tests like CSF oligoclonal bands, visual evoked potentials, optical coherence tomography, and autoantibody tests for AQP4 and MOG are used when presentations are atypical or insufficiently conclusive.
Clinical Presentation and Diagnosis of RRMS
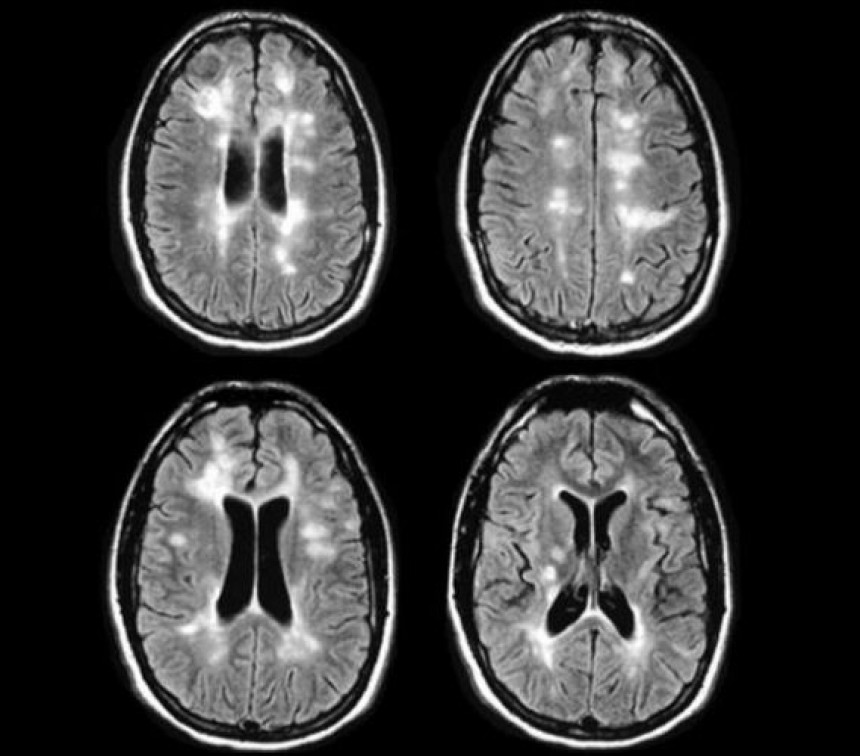
Relapsing remitting MS (RRMS) is primarily a clinical diagnosis. There are no clinical findings which are unique to RRMS. Typically, patients present as young adults with one or more episodes of central nervous system (CNS) dysfunctions. Common CNS manifestations include unilateral visual loss, diplopia, sensory loss in limbs, motor weakness in limbs, gait disturbance and balance disorders. Typical findings on MRI include hyperintense white matter lesions (plaques) on T2 sequences in characteristic locations (periventricular, cortical, infratentorial and the spinal cord). Patients typically have recovery after attacks. (1, 2)
McDonald Diagnostic Criteria for RRMS
McDonald diagnostic criteria for RRMS include the following; If patients have a history of two or more attacks and have objective clinical evidence of two or more lesions, then, the diagnosis of RRMS is clear with no additional investigation required. For patients with a history of two or more attacks who have objective clinical evidence of only one lesion, the criteria require additional evidence from either, MRI (MS lesions in at least two of four MS typical regions of the CNS) or by the development of an additional clinical attack which implicates a different CNS region. (3)
Diagnostic Testing for Atypical Presentations of RRMS
For patients with typical presentation who have insufficient clinical and radiological evidence, additional testing with cerebrospinal fluid (CSF) specific oligoclonal bands, visual evoked potentials and/ or optical coherence tomography are required to support the diagnosis. Finally, for patients with an atypical presentation, additional testing with spinal MRI, lumbar puncture, and/or autoantibody checking for aquaporin-4 (AQP4) and myelin-oligodendrocyte glycoprotein (MOG) is warranted. (3, 4, 5)
CSF Assessment in RRMS
Qualitative assessment of CSF for oligoclonal IgG bands using isoelectric focusing is the most important CSF study in RRMS. (6)
Visual Evoked Potential in RRMS Diagnosis
Visual evoked potential is used to detect abnormal visual function and to define lesions in optic nerve/ tract not easily visualised by imaging. (7)
Role of Optical Coherence Tomography (OCT) in RRMS
Optical coherence tomography (OCT) uses infrared light waves which visualise the internal microstructure of biological tissues based on the differential optical reflectivity. It can be used to measure the thickness of the retinal nerve fibre which is reduced in most patients with optic neuritis. (8)
Autoantibody Testing in RRMS
Testing for the aquaporin 4 (AQP4) IgG serum autoantibody and the myelin oligodendrocyte glycoprotein IgG autoantibody (MOG) IgG are indicated for patients presenting with acute CNS demyelination when clinical, imaging or other laboratory features are atypical for the diagnosis of RRMS. (9, 10)
References
1-van der Vuurst de Vries RM, Mescheriakova JY, Wong YYM, et al. Application of the 2017 Revised McDonald Criteria for Multiple Sclerosis to Patients With a Typical Clinically Isolated Syndrome. JAMA Neurol 2018; 75:1392.
2-Filippi M, Rocca MA. MR imaging of multiple sclerosis. Radiology 2011;
259:659.
3-Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–17.
4-Filippi M, Preziosa P, Banwell BL, et al. Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines. Brain 2019; 142:1858.
5- Rosati G. The prevalence of multiple sclerosis in the world: an update. Neurol Sci. 2001;22:117–39
6-Pohl D, Rostasy K, Reiber H, Hanefeld F. CSF characteristics in early-onset multiple sclerosis. Neurology 2004; 63:1966.
7-Giesser BS. Diagnosis of multiple sclerosis. Neurol Clin 2011; 29:381.
8-Petzold A, de Boer JF, Schippling S, et al. Optical coherence tomography in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol 2010; 9:921.
9-Jarius S, Paul F, Aktas O, et al. MOG encephalomyelitis: international recommendations on diagnosis and antibody testing. J Neuroinflammation 2018; 15:134.
10-Ramanathan S, Dale RC, Brilot F. Anti-MOG antibody: The history, clinical phenotype, and pathogenicity of a serum biomarker for demyelination. Autoimmun Rev 2016; 15:307.





