Spontaneous Intracranial hypotension
Spontaneous intracranial hypotension (SIH) is a condition characterized by symptoms such as orthostatic headache, low cerebrospinal fluid (CSF) pressure, and diffuse meningeal enhancement on brain MRI. The condition often presents with a normal neurological examination and can include other symptoms related to low CSF pressure. The diagnosis and management of SIH involve specific imaging techniques and a range of treatments from conservative approaches to surgical interventions.
Overview of Spontaneous Intracranial Hypotension
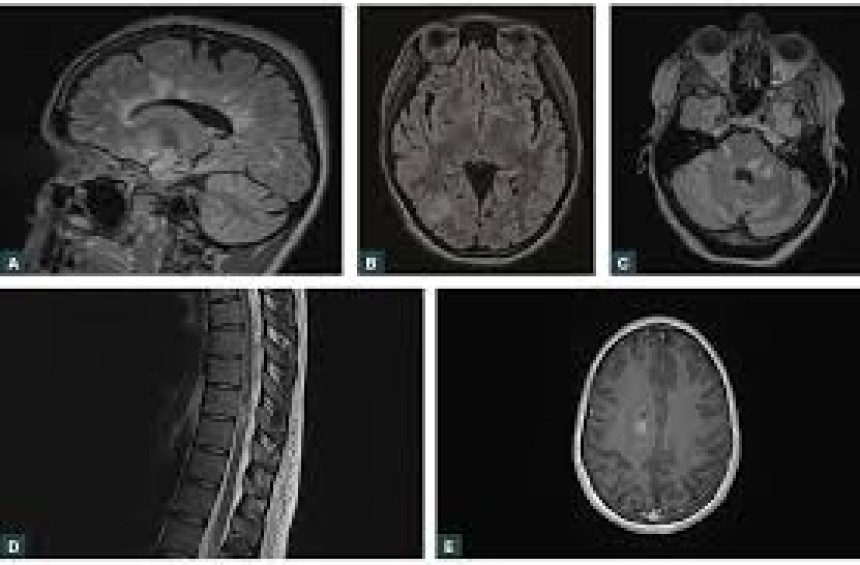
Spontaneous intracranial hypotension is a syndrome which includes orthostatic headache, low cerebrospinal fluid (CSF) pressure, and diffuse meningeal enhancement on brain magnetic resonance imaging (MRI). Occasional patients report no headache, typically when other symptoms of low CSF pressure are predominant.
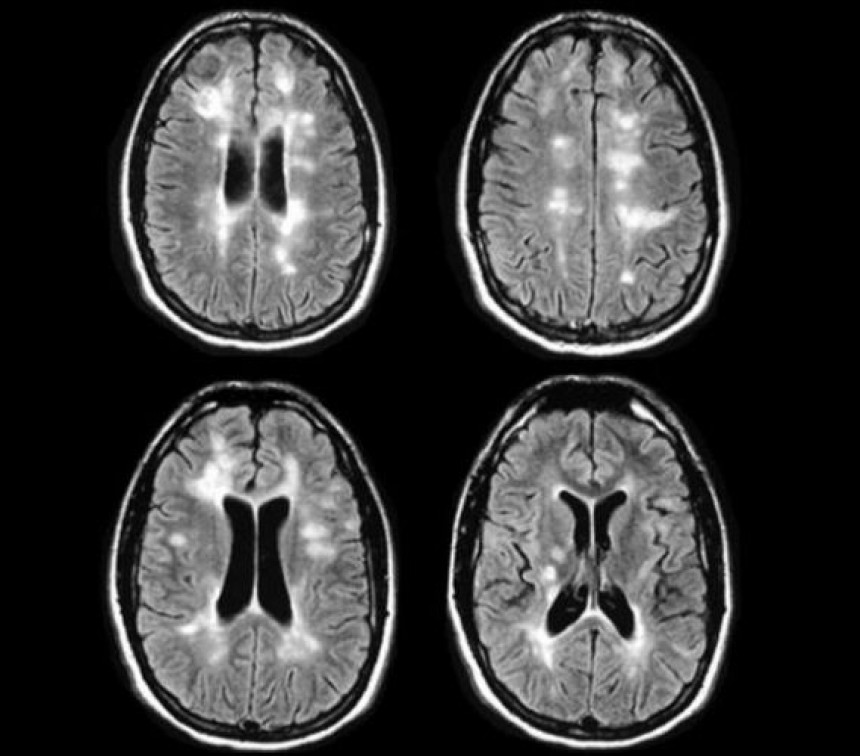
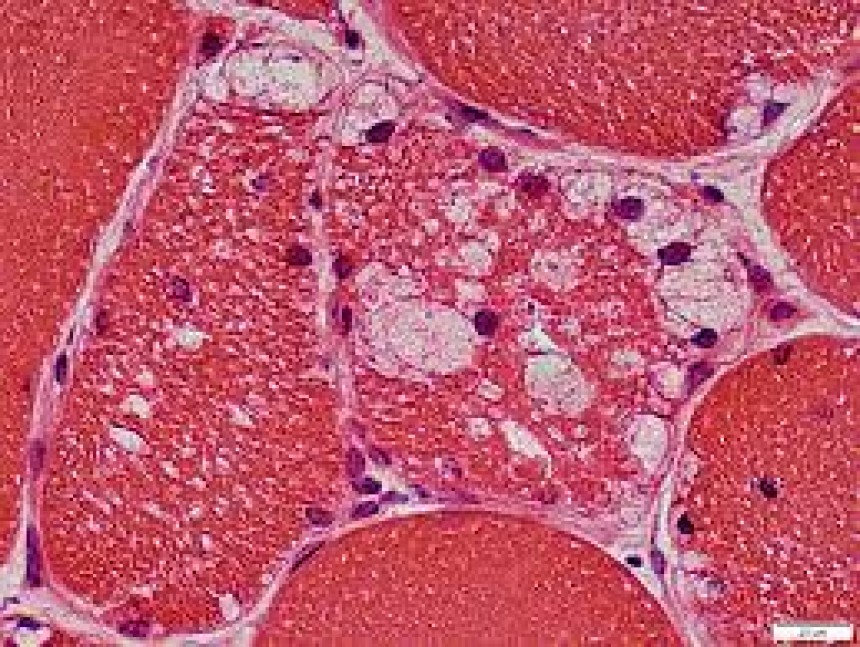
Neurological Examination and Imaging
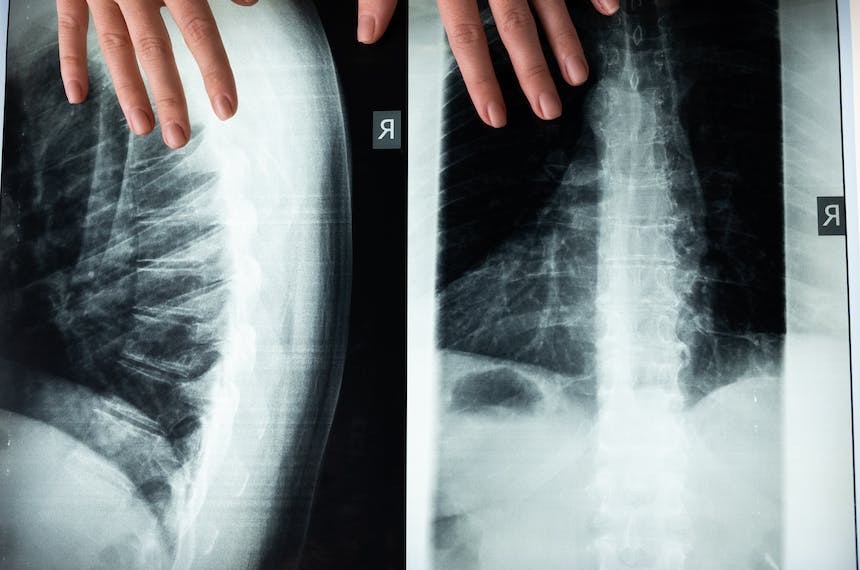
The neurological examination is often normal in patients with spontaneous intracranial hypotension. Brain MRI and spinal MRI are advisable to assess for the typical imaging features of the syndrome.
Conservative Treatment Approach
Patients with acute uncomplicated mild to moderate headache can be treated initially with conservative therapy including avoidance of the upright position, strict bed rest, oral or intravenous hydration, high oral caffeine intake, high salt intake, and the addition of analgesics.
Epidural Blood Patch (EBP) for Severe or Longstanding Cases
Patients with severe or longstanding headache should be treated initially with an epidural blood patch (EBP), which represents the mainstay treatment of the disease.
Mechanism and Procedure of EBP
The mechanism for the success of EBP is believed to involve tamponade of the dural leak and later fibrin deposition and scar formation. The initial EBP treatment typically involves the infusion of autologous blood into the epidural space.
Additional Treatment Options for Refractory Cases
For patients who fail conservative therapy and repeated EBP treatments, options include continuous epidural saline infusion, epidural fibrin glue, or surgical repair of the defect. Localization of CSF leaks is usually done with CT myelography or radioisotope cisternography.
References
- Lay CL, Campbell JK, Mokri B. Low cerebrospinal fluid pressure headache. In: Headache, 1997. p.355.
- Mokri B. Low cerebrospinal fluid pressure syndromes. Neurol Clin. 2004;22:55–74.
- Schievink WI, et al. Spontaneous intracranial hypotension in childhood and adolescence. J Pediatr. 2013;163:504–10.
- Williams EC, et al. Spontaneous intracranial hypotension: presentation, diagnosis, and treatment. Anesthesiology. 2014;121:1327–33.
- Lin W, Geiderman J. Myth: fluids, bed rest, and caffeine in post-lumbar puncture headache. West J Med. 2002;176:69–70.
- Madsen SA, et al. Epidural blood patch for refractory low CSF pressure headache. J Headache Pain. 2011;12:453–7.
- Schievink WI, et al. Treatment of spontaneous intracranial hypotension with percutaneous fibrin sealant. J Neurosurg 2004; 100:1098.